6-Part EMT Core Content Guide
6-part study guide for EMT to help you study the most important things in a reasonable time frame.


From anaphylaxis to soft tissue injury, our pathophysiology-focused guides ensure you know critical information for the NREMT.

From anaphylaxis to soft tissue injury, our pathophysiology-focused guides ensure you know critical information for the NREMT.
This outlines how to use the resources on EMTReview.com and in your textbook, with exercises that train you in the critical thinking skills needed for the NREMT.
These cover challenging topics like respiration, acid base and ETCO2, shock and fluid resuscitation, and pharmacology. Each includes a separate answer key with detailed rationales.
6-part study guide for EMT to help you study the most important things in a reasonable time frame.

5 study guides designed to tackle the most comprehensive and challenging facets of the paramedic curriculum.

Key concepts in medical math for paramedics.

All of our content is written and reviewed by national EMS experts, including textbook authors, speakers, and former NREMT personnel.

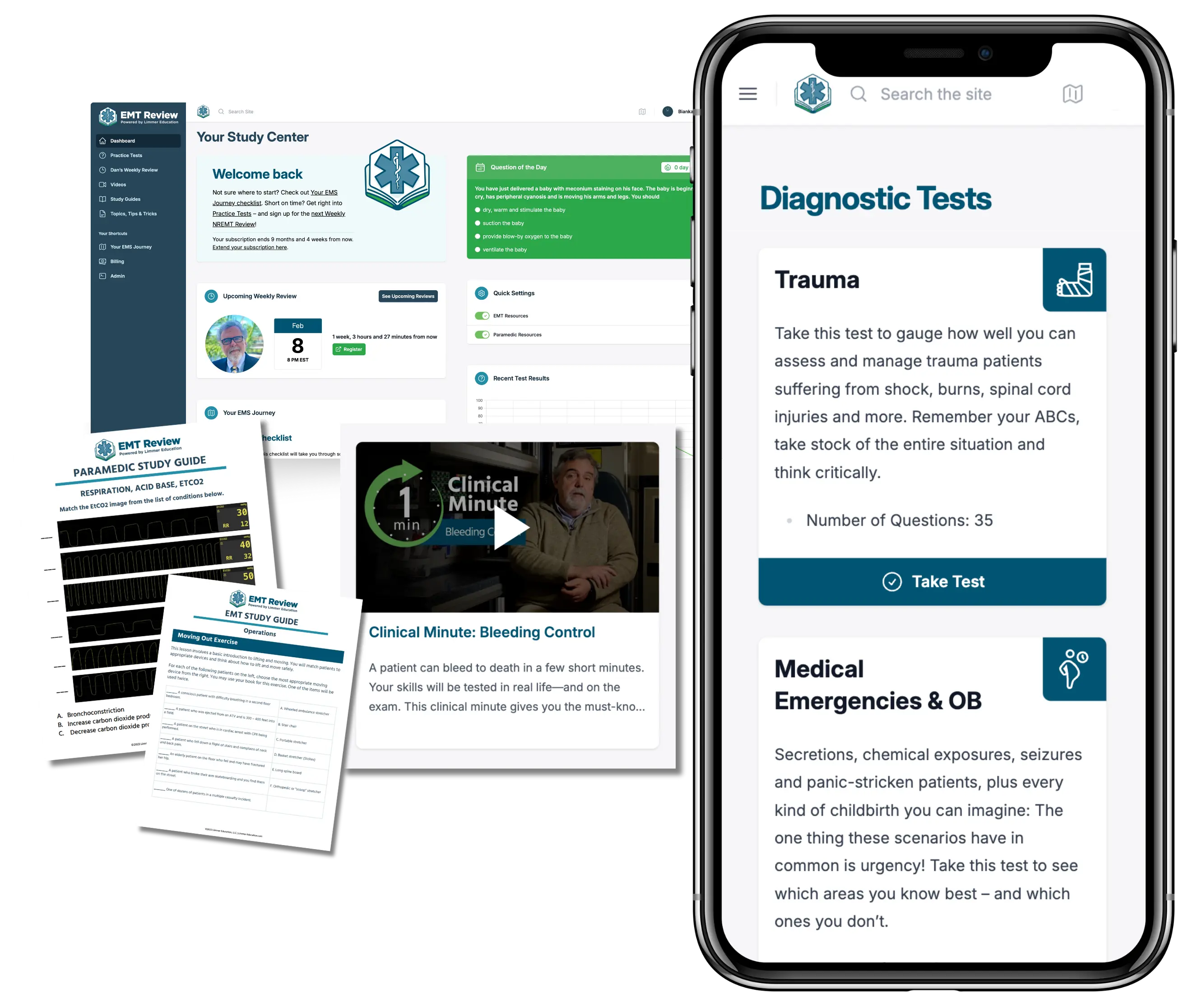
The most in-depth, most affordable NREMT test prep available! Practice tests, videos, study guides, live reviews, and so much more.
Join Now